Eur Respir J Published online 17 December, 2020 | https://doi.org/10.1183/13993003.02828-2020
Digest author: Sarah Cullivan, MD / 14 February, 2021
The ERS statement on chronic thromboembolic pulmonary hypertension (CTEPH) provides a comprehensive overview of CTEPH, summarising current knowledge and highlighting important research questions.
CTEPH is a rare and underrecognised complication of acute pulmonary embolism (PE), that is characterised by persistent intravascular fibrotic occlusions of pulmonary arteries and a secondary microvasculopathy of smaller vessels. If left untreated this can result in increased pulmonary vascular resistance and right ventricular (RV) afterload and right heart failure.
Echocardiography is the test of choice to screen for pulmonary hypertension (PH) post PE, following at least 3 months of effective anticoagulation. Ventilation/perfusion (VQ) scintigraphy is recommended to assess for mismatched perfusion defects, suggesting failure of clot resolution, though this statement recognises the evolving role of additional imaging modalities such as VQ SPECT. Further vascular imaging and right heart catheterisation (RHC) are then required to confirm a diagnosis of CTEPH. The proposed change to the haemodynamic definition of PH, lowering the mean pulmonary artery pressure threshold from ≥25 mmHg to >20 mmHg, will presumably have implications for the diagnosis of CTEPH. In the absence of PH, the term CTEPD (chronic thromboembolic pulmonary disease) is now preferred to CTED (chronic thromboembolic disease).
The estimated prevalence of CTEPH in the general population ranges from 19 to 50 per million, and the cumulative incidence from 0.1 to 11.8% in the first two years following symptomatic PE. A number of risk factors for the disease are recognised, including permanent intravascular devices such as pacemakers, inflammatory bowel disease and essential thrombocythaemia. Further research is required to clarify the
natural history of the disease, to identify biomarkers of fibrotic thrombus transformation and to define the role of targeted screening in high risk populations post PE.
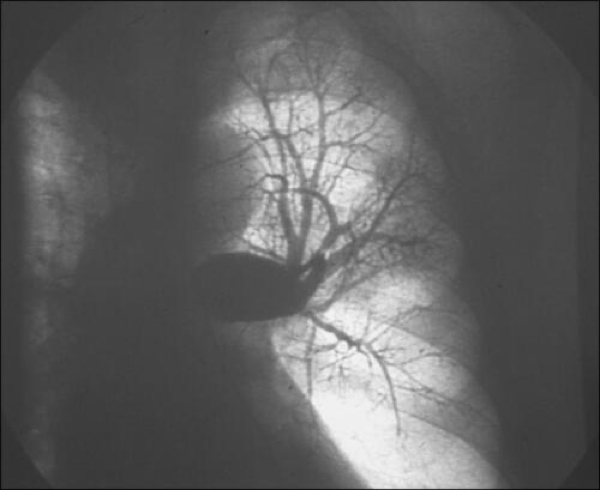
Two types of vascular lesions are described in CTEPH; fibrotic obstructing lesions in proximal pulmonary arteries and a distal microvasculopathy in vessels less than 500 µm. Lifelong anticoagulation is recommended for all patients with CTEPH. While vitamin K antagonists have historically been the drug of choice in CTEPH, novel oral anticoagulants are increasingly used and appear to be safe in most cases, except in triple positive antiphospholipid syndrome. Treatment of CTEPH often employs different treatment modalities, and available options include medical therapies, such as the soluble guanylate cyclase stimulator (sGCS) riociguat and/or the prostacyclin analogue treprostinil, balloon pulmonary angioplasty (BPA) and pulmonary endarterectomy (PEA). PEA is the treatment of choice for operable CTEPH, and both PEA and BPA should be performed in expert, high volume centres, with adequately trained surgeons and interventionalists. While surgery may improve and even normalised pulmonary haemodynamics, it is unlikely to return all pulmonary vessels to normal and therefore a ‘cure’ may not be obtained in many cases. Rehabilitation in CTEPH is important, effective and safe and should be a focus of future studies.
This statement represents a summary of current knowledge of CTEPH and highlights important unanswered questions, that should guide future research in the field.