The impact of COVID-19 on patients with Interstitial Lung Disease (ILD) was studied in this international multicentre audit. Outcomes in exacerbations of IPF have a mortality rate ranging from 35-70% and the impact of COVID-19 infection was not known.
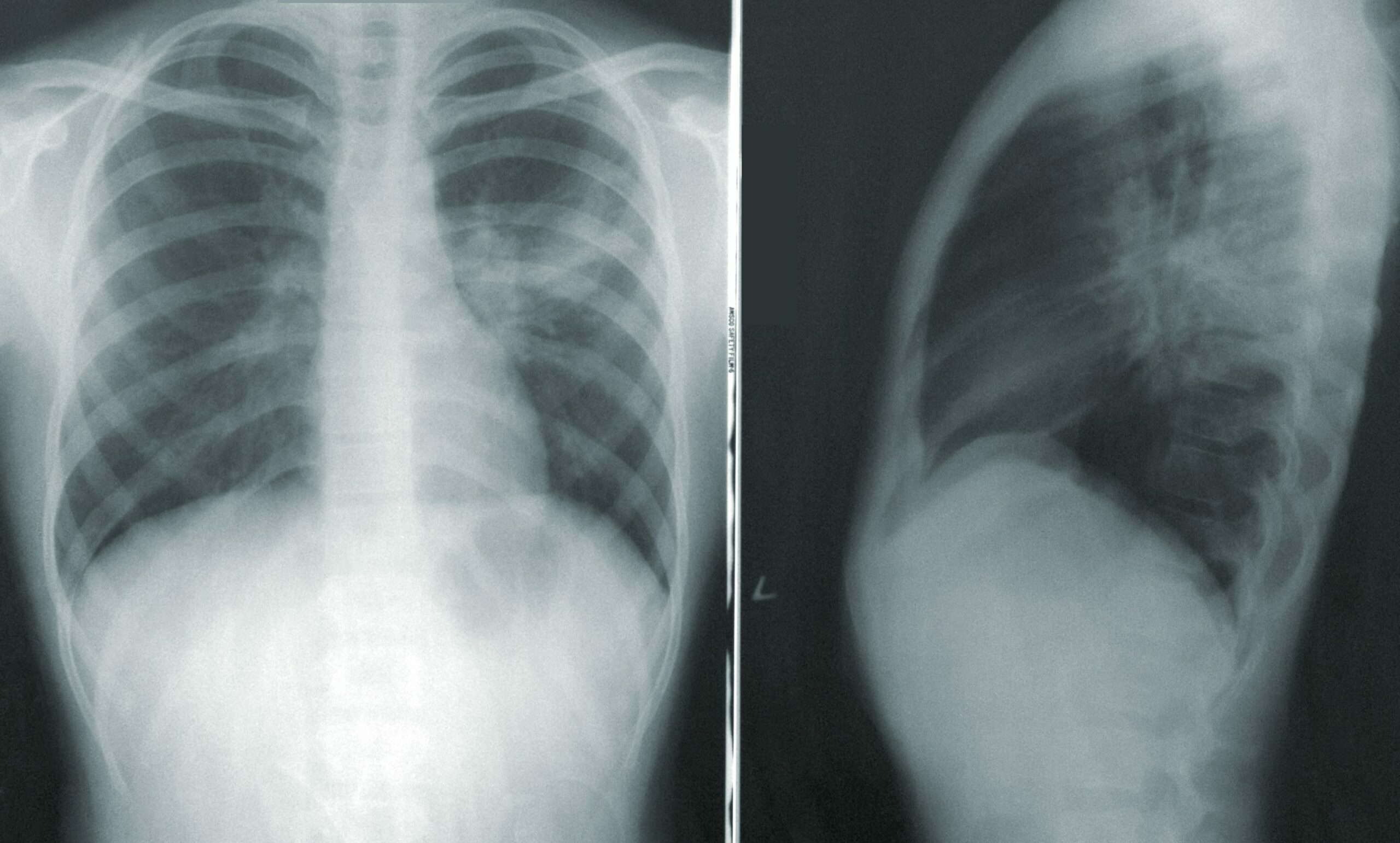
This was an international multicentre analysis of ILD patients admitted to hospital between March 1 and May 1 2020 with COVID-19. This was facilitated through reaching out to physicians involved in ILD care through research networks including centers in Denmark, Germany, Italy, Republic of Ireland, Spain and UK. Diagnosis of SARS-CoV-2 was based on positive PCR swab and / or clinicoradiological diagnosis. The ISARIC4C CCP-UK database was used to provide comparison of COVID-19 patients without ILD.
The primary outcome was in-hospital mortality. Secondary outcomes included whether patients received “enhanced respiratory support” (mechanical or non-invasive ventilation or high-flow oxygen).
Over the 2 month period, 349 ILD patients were admitted to 37 hospitals. There were 185 patients with ILD and COVID-19. IPF was the most common ILD. During the same period 164 patients were admitted with an alternative non-COVID diagnosis, of whom 69 (42.1%) had IPF. In-hospital mortality for ILD and COVID-19 was 49% compared with 17% for patients with ILD / non-COVID.
There was significantly higher mortality in patients with ILD than in those without ILD (49% vs 35%) and ILD was associated with an increased risk of death in a matched adjusted analysis (p=0.013). This was greater in men, increased age and obesity. Survival was significantly poorer in IPF patients but also in non IPF ILD. In the non-IPF ILD group chronic hypersensitivity pneumonitis and rheumatoid ILD had the highest mortality whereas sarcoidosis and connective tissue disease (excluding rheumatoid) related ILD had the lowest mortality.
Survival was significantly poorer in patients with moderate or severe ILD (FVC < 80%) than in patients with mild disease (FVC> 80%) (HR 1.72).
Most patients with ILD (84%) did not receive enhanced respiratory support, similar to matched patients without ILD. Of the 26 patients receiving enhanced respiratory support 77% (20) died including 83% (5/6) of matched patients with ILD receiving ventilation. Immunosuppressants or antifibrotic therapy was not shown to affect mortality.
Comment:
- This information is important in guiding treatment and education of ILD patients and also in assessing prioritisation of groups for vaccination.