Increased variation in the lung function of cystic fibrosis (CF) patients is a significant predictor of poor adherence to prescribed medication, according to new research published in the ERJ.
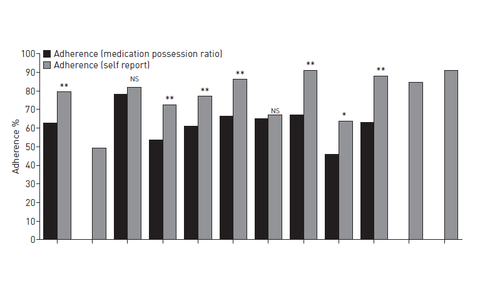
Researchers collected data from 249 CF patients registered with a large CF health unit; participants were over 16 years of age and had a diagnosis of CF. Adherence to prescription medication was measured based on a composite medication possession ratio (MPR) score combined with self-report data.
A physiotherapist recorded forced expiratory volume in 1 s (FEV1) and forced vital capacity (FVC) for 12 months and used the best value from a series of at least three attempts. The total, mean and standard deviation of all values for FEV1 for each participant were calculated.
The coefficient of variation (CoV) for FEV1 was calculated by extracting all consecutive highest then lowest values for FEV1 for 6 and 12 months prior to baseline; these timescales aligned closely to pharmacy medication records.
The results showed that patients with poor adherence to medication prescriptions had on average a 4.67% higher CoV for FEV1, and a 7.3% higher CoV CRP compared with those with good adherence, which suggests that poor adherence can make CF patients more prone to fluctuations in lung function.
The researchers also found that a significant predictor of adherence in the overall models was the number of medications prescribed; as adherence improved from ‘poor’ to ‘good', the number of medications taken daily by CF patients increased.
The authors believe this is the first study to demonstrate a significant inverse relationship between CoV FEV1 and adherence to treatment in adults with CF, but conclude that this novel marker of adherence requires further evaluation across treatment regimens and duration of treatment.